Surgery & Surgical Menopause
Surgery is the last line in treatment for premenstrual disorders, reserved for those who have not gained relief through other evidence-based treatments.
It involves the removal of the ovaries and often the uterus, which induces menopause and is called surgical menopause. There are many factors to weigh when considering surgical menopause as a treatment for PMDD/PME, including medical eligibility, the likelihood of treatment success, and personal preferences. While there is a lot of information online about menopause, it can be hard to find information about surgical menopause, especially for those with PMDD/PME, hormone sensitivity disorders.
With financial assistance from She+ Foundation, we have created this comprehensive extension to our website on surgical menopause for PMDD. Here, you'll find helpful information when considering, preparing for, and recovering from surgery and tools to help you thrive in surgical menopause.
Surgery: The Basics
-
Surgical menopause (sometimes called surmeno) is a surgically induced menopause that refers to the menopausal (low) hormone state that occurs following surgical removal of both ovaries. This procedure is called a bilateral oophorectomy and is the last line of treatment for PMDD/PME when less invasive treatments have not been effective.
A unilateral oophorectomy involves removing just one ovary (leaving the other). This does not result in surgical menopause, and the remaining ovary continues to produce normal hormone cycling each month.
Sometimes, a surgical removal of the uterus (a hysterectomy) is performed at the same time as removal of your ovaries (oophorectomy) due to an intolerance to progestogen add-back. If you have a hysterectomy but keep your ovaries, you will not experience a surgical menopause - your hormones will continue to cycle as they usually would each month, even though your uterus is gone (and you will have no menstrual bleeding). A hysterectomy without ovary removal is not a treatment for PMDD.
-
The essential part of the surgical procedure is the removal of both ovaries (bilateral oophorectomy or bilateral salpingo-oophorectomy if the fallopian tubes are also removed). PMDD is a severe adverse reaction in the brain to the natural rise and fall of estrogen and progesterone, triggered by ovulation, a process that takes place in the ovaries. By removing the ovaries (when all other forms of cycle suppression have not worked), you remove ovulation and thus, remove those fluctuations from happening.
Pre-Surgery (Fluctuations)
At a basic level, PMDD is caused by a sensitivity in the brain to the natural hormone fluctuations that occur as part of the menstrual cycle. The brain has an adverse reaction to those ups and downs of the ovarian hormones.
Post-Surgery (Steady Levels of Hormones)
By removing the ovaries, and therefore removing ovulation/the menstrual cycle, and using hormone replacement therapy (HRT) to keep the estrogen and progesterone levels even and steady, you eliminate the fluctuations that trigger PMDD symptoms.
-
When discussing surgery for PMDD, you will often hear people talking about having a hysterectomy, which can cause lots of confusion and misunderstanding. When surgical menopause is used as a final treatment for PMDD, the removal of the ovaries is the critical part of the treatment since the ovaries cause hormone fluctuations, and therefore trigger PMDD.
The type of surgery you need depends on if you tolerate the progesterone add-back in hormone replacement therapy.
Bilateral Oophorectomy: If progesterone add-back is tolerated, then you may only need a bilateral oophorectomy, which is the surgical removal of both ovaries. Your surgeon may suggest the removal of fallopian tubes as well, which is referred to as Bilateral Saplingo-Oophorectomy (BSO). Because your body needs some hormones to stay healthy, the doctor will usually prescribe stable continuous doses of estrogen for bone and heart health, and progesterone to prevent uterine cancer risks.
Total Hysterectomy and Bilateral Saplingo-Oophorectomy (THBSO): If progesterone add-back is NOT tolerated, then you would need a Total Hysterectomy and Bilateral Saplingo-Oophorectomy. This would involve the removal of the urterus, both ovaries and both fallopian tubes. Removing the uterus can help avoid the risk of excess build up of cells or tissue when using estrogen-only therapy.
-
Surgery for a premenstrual disorder is a big decision with lifelong impacts on the body. Removing your ovaries is an invasive procedure that immediately causes surgical menopause and menopause symptoms. The decision to have surgery is not made lightly. However, when someone with PMDD/PME has ruled out all other evidence-based treatments and still suffers severe symptoms that keep them from functioning in their everyday life, surgery can be a life-changing, effective treatment.
“SSRIs worked quite well for me in my 20s and made my symptoms pretty manageable for a long time. However, in my 30s, my symptoms severely worsened, and despite working my way through the available treatment options, nothing worked (and often made me feel worse). It took me a while to get my head around the fact that surgery could be an option. I read lots of blogs and joined groups. At the end of the day, I felt like I was out of options and wanted my life back.” —Patient
Essentially, surgery for a premenstrual disorder is the last treatment option when your symptoms are severe and no other interventions have worked.
Having surgery at a younger age for severe PMDD? Listen to this podcast where IAPMD Volunteers Rachel & Anna share their experiences of having surgery in their early 20s.
-
Symptoms of surgical menopause are caused by estrogen deficiency. Following the surgical removal of the ovaries, you become post-menopausal immediately. As your hormone levels drop, you may experience a sudden onset of menopausal symptoms. These may be mild, moderate, or severe. These symptoms can be minimized by taking Hormone Replacement Therapy (HRT), or alternatives (see estrogen alternatives here) if hormones are not an option following surgery.
Symptoms include, but are not limited to:
Vasomotor symptoms (e.g., hot flashes/flushes and sweats)
Musculoskeletal symptoms (e.g., joint and muscle pain)
Effects on mood or anxiety (e.g., feeling abnormally sad or worried)
Urogenital symptoms (e.g., vaginal dryness, needing to urinate frequently)
Sexual difficulties (e.g., low sexual desire, painful sex)
Other (e.g., headaches, sleep issues, skin changes)
Menopausal symptoms, as a result of estrogen deficiency, can also be long-term, but individual experiences vary. HRT can reduce these symptoms and can be safely taken long-term, except in some circumstances.
Long-Term Health Risks
The ultra-low levels of estrogen in surgical menopause can cause bothersome menopausal symptoms. Still, more importantly, they can reduce the length and quality of your lifespan by increasing the risk of various health conditions. We will address each below.
For those under the age of 40 who enter surgical menopause, using HRT (Hormone Replacement Therapy) can reduce or eliminate the serious long-term health risks associated with surgical menopause, including:
Osteoporosis and broken bones
Cardiovascular Disease (e.g., heart attack, stroke)
Dementia and Parkinson’s Disease
Psychiatric Disorders (e.g., mood or anxiety disorders)
Vulvar and Vaginal Atrophy
Sleep Disorders (e.g., persistent and impairing insomnia)
Higher risk of death by any cause
To summarize, surgical menopause is known to cause all of the above symptoms and health risks. Still, these problems can generally be reduced or eliminated by using estrogen therapy following surgery through to the typical age of menopause (51 years).
Most individuals in surgical menopause choose to continue some level of estrogen through at least age 60 to maintain symptom relief.
-
Natural Menopause
Natural menopause occurs when the ovaries stop releasing eggs, and as a result, the levels of sex steroid hormones (estrogen, progesterone, and testosterone) fall. The average age of natural menopause is 51, but any time after 45 is considered “normal.”
The years during the menopausal transition are called perimenopause, which can last months or even up to years. Periods often become heavier and more sporadic during this time, and menopausal symptoms (e.g., night sweats, hot flashes, or vaginal dryness) begin to appear. If you are going through menopause naturally, you will be considered postmenopausal a year to the day of your last period. If menopause occurs between the ages of 40 and 45, this is referred to as early menopause. One in a hundred women will experience menopause under the age of 40. This is referred to as premature menopause or premature ovarian insufficiency (POI).
Surgical Menopause
In those who undergo a bilateral oophorectomy (removal of both ovaries), the transition into menopause is immediate and known as surgical menopause. Surgical menopause symptoms can be sudden and may be more intense than those experienced in natural menopause, especially in younger individuals. It can be unpleasant or distressing, so working with an experienced healthcare professional to look after both your short-term and long-term health during this rapid transition is essential.
-
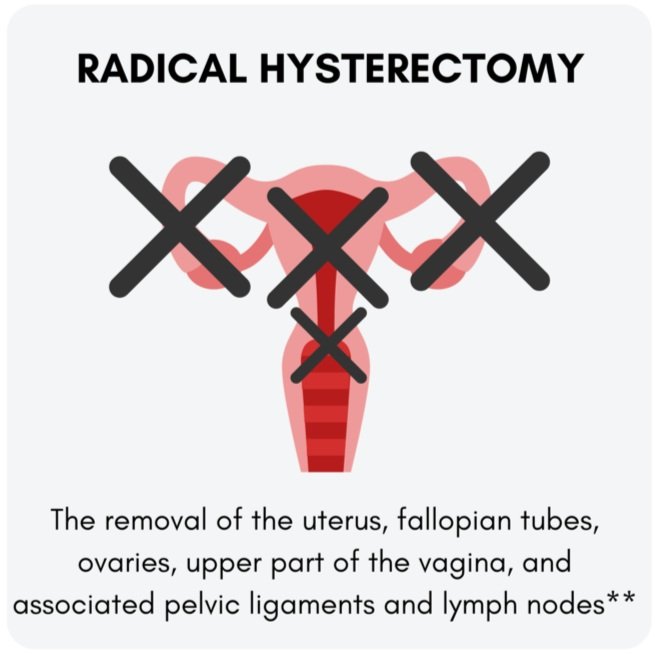
The following surgical procedures will result in surgical menopause, as illustrated below:
*The cervix may also be removed depending on the individual’s reaction to HRT in both THBO and THBSO surgeries.
**A radical hysterectomy is typically performed when someone has cancer of the cervix, ovaries, fallopian tubes, or uterus. It is not a standard treatment for PMDD/PME.
Considering Surgery
While living with a premenstrual disorder can make us feel desperate for relief, surgery for PMDD needs to be a well-considered decision. It is reserved for those who have not gained relief through the evidence-based treatments.
-
Surgical menopause is not an easy treatment to access for most people with PMDD. There are many reasons for this, not least of which is that PMDD is a relatively new diagnosis (created in 2013), and many providers have little experience working with the disorder. Among providers who do approve surgery for PMDD, the following criteria (1 & 2) usually need to be met before they will consider moving forward with more invasive treatments.
Am I medically eligible? How do I know whether a doctor will consider referring me for surgery?
Eligibility
-
Physicians who make decisions about surgical eligibility generally require a PMDD patient to have two months of daily symptom ratings (that are detailed recordings/tracking of your symptoms alongside your cycle) that show a pattern consistent with PMDD before considering advanced treatments such as chemical or surgical menopause.
To be eligible for more invasive treatments, such as surgical menopause, symptoms should cause significant life impairment. It can be helpful to make notes in your daily ratings about how much your symptoms impact your ability to work, care for yourself, parent, and maintain relationships. It is also helpful to document any inpatient hospitalizations and note if they have occurred due to PMDD.
-
All physicians take an oath to “not harm” with their treatments, and they never want to expose people to greater physical risk due to their treatments. Since surgery brings more significant physical risks than most other medical treatments, surgeons making decisions about surgical treatment of PMDD are often quite concerned about whether they might be “harming” you by approving surgery, and about whether they will be held responsible if the surgery does not work for you. Because of this, your doctor will want to ensure that you have tried all other options before going under the knife.
To document this, surgeons often require that you gather medical records showing that you’ve tried several of the less-invasive first-line treatments that have been shown to work better than a placebo (inactive treatment) in clinical trials for PMDD. This includes documenting the use of SSRIs and drospirenone-containing oral contraceptives, and that you still experience unmanageable symptoms despite these treatments.
It is also a good idea to continue to use daily ratings (tracking your symptoms daily) as noted above to document how symptoms change (or do not change) in response to these treatments.
As part of this process, doctors often also try to treat other co-occurring disorders that you may have in addition to PMDD, such as major depressive disorder (MDD) or generalized anxiety disorder (GAD). If they do this, rest assured that they are not saying that you don’t have PMDD-- they are trying to reduce your suffering overall by tending to these other, more chronic symptoms that may worsen or complicate PMDD.
-
If approved by your physician, you will also need to complete an assessment visit with the surgeon to review your other medical history and make sure that the advanced treatments that cause a menopausal state are safe for you. Some individuals may be unable to undergo surgery safely, which needs to be evaluated during this process.
-
Before a doctor decides to move forward with surgical intervention for PMDD, they usually want to use temporary medications to “test out” menopause, before moving on to surgery.
The reason that surgical menopause is effective for PMDD is that it eliminates cyclical hormone changes, which prevents the hormone-sensitive (PMDD) brain from having adverse cyclical PMDD reactions. To test whether surgical menopause will be an effective treatment for you, it is wise to test out how you will respond to a menopausal hormone state. The best way to test out whether a menopausal state is right for you is to undergo a “reversible chemical menopause trial,” in which medications called “GnRH analogues” are given to shut down your ovaries temporarily (which stops your hormones from fluctuating). It is fully reversible-- once you decide to stop the medication, your hormones will resume cycling as normal. If symptoms go away or improve vastly during this temporary “reversible chemical menopause trial”, this is a sign that surgical menopause may be a treatment option for you.
Note that not all doctors require this, but most do. If, for some reason, these medications do not successfully prevent ovulation and you continue to have hormone cycling (and symptoms), you and your doctor may still decide that surgery is the right option.
Generally speaking, surgeons become much more comfortable with the prospect of surgical treatment for PMDD once the four points above have been addressed.
Other Considerations
-
Of course, your preferences and personal situation are significant in deciding. We understand that many people with PMDD/PME are desperate to escape the relentless cycle of PMDD/PME. It is essential to realize that this surgery is a significant and irreversible decision. It will be life-changing. The decision to undergo such major surgery must be thoroughly thought through by you and made with your doctor/health-care provider.
All risks and benefits of the surgery (and life following the surgery) should be explained to you in full.
If you would like to talk to others in your situation, you can join our Facebook peer support group, IAPMD—PMDD, Oophorectomy, Hysterectomy, & Life After Group.
-
It is important that you learn about the procedure and what it means for your health in the long term. This will allow you to make a decision based on your personal situation.
For some, it can be helpful to arrange talk therapy to discuss your options and give you time to make a decision on your own terms and within your timeframe.
You should not agree to this surgery unless you understand the reasons for it and the pros and cons of having your ovaries removed. If you are unsure about anything, ask your doctor or healthcare provider for clarification or further information.
-
You will know you are progesterone intolerant if you have an adverse psychological reaction (and in some cases, adverse physical reactions also) to taking progestin-based medications. Examples of these medications are:
Combined contraceptive pill
POP (progesterone only pill)
Hormonal IUD/coil such as the Mirena/Jaydess.
Oral micronized progesterone
Depo Progesterone injection or the Implanon.
Note that there is a difference between progestins like those in hormonal birth control and naturally occurring progesterone formed in the human body.
“Within days of taking any progesterone product, the drop in mood and mood swings started. I came off it, and they went away. This was repeated several times with several different products.” —Patient
Micronised Progresterone
Micronised progesterone (such as Prometrium or Utrogestan) is identical to the progesterone made in the human body, and, for many, has fewer side effects than the progestins found in birth control pills.
In either case, studies have shown that it is often the change in progesterone-- and not the level of progesterone itself-- that triggers symptoms of “progesterone intolerance” in PMDD. It may be that, once the brain has had time to adjust to the new level of progesterone metabolites (typically one month), the symptoms will go away.
-
There are short-term and long-term risks associated with surgical menopause, and you need to fully understand these before going ahead with surgery.
Surgical Risks
Any surgery has risks, including, for example, a reaction to the anaesthetic, bleeding, infection, or pain after the procedure. Your surgeon will explain these to you before your surgery, before you sign the consent form. It is essential to understand that surgery will only go ahead if the benefits are believed to outweigh any risks.
Psychological Effects of Surgery
While everyone’s experience is different, some people may feel emotionally upset immediately following surgery. PMDD is a sensitivity to hormone fluctuations, and after surgery, your hormone levels drop significantly, thus making it a difficult time for many people. Ensuring those around you understand why you are having the surgery and having a good support network is very important.
Surgery and surgical menopause are significant physical and psychological adjustments for anyone, and this should not be underestimated.
Estrogen Deficiency-Related Menopause Symptoms
Following surgical removal of the ovaries, you become post-menopausal immediately. As your hormone levels drop, you may experience a sudden onset of menopausal symptoms. Depending on your situation, these may be mild, moderate, or severe. These symptoms can be minimized by taking Hormone Replacement Therapy (HRT) or alternatives if hormones are not an option following surgery.
Preparing for Surgery
Preparing for surgery can feel like an emotional roller coaster. It’s normal to have questions, doubts, or moments of uncertainty—“Am I making the right decision?” You’re not alone. Many have walked this path before and faced the same worries and emotions.
This section offers guidance on how to prepare—both emotionally and practically—for what lies ahead.
-
Going to the pre-op appointment can be daunting, and many people worry as they do not know what to expect if they have not had surgery before.
The pre-op appointment helps everyone prepare you safely for your procedure or operation and identify areas where you can improve your general health before anaesthesia. For the hospital to safely assess your suitability for the surgery, they will need to learn about your medical and surgical history, any medication (and supplements) you are taking, and any previous medical issues.
On the day of your appointment, it may be helpful to bring with you:
A written list or prescription of your medications (and supplements)
A list of your previous operations or illnesses (do not worry if you cannot recall the exact dates)
Any previous copies of hospital doctors’ letters, if you have them available
Your contact details and details of your doctor(s)
Write down any questions or concerns you have. It can also help to take some paper and a pen to jot down answers at the time, as it is easy to forget the details.
Upon arrival at the clinic, you will be asked to confirm your name, address, contact details, and GP details.
In your appointment, a healthcare assistant will make routine observations such as your height, weight, blood pressure, and heart rate (ECG). You may also have some routine skin swabs taken, and some patients may also require a urine sample.
You will usually have a consultation where a healthcare provider will take a detailed medical history from you. The whole assessment usually lasts under an hour. However, it may run a little longer if you have a complicated medical history and/or need additional tests.
📌 Tip: Each hospital has its own way of doing things. If you are particularly nervous, call ahead and ask them to explain what is covered at a pre-op. Many hospitals also have details on their website, so you can look them up ahead of time to calm your nerves.
-
Laparoscopic Surgery
How it works
A small tube containing a telescope (laparoscope) and a tiny video camera will be inserted through a small cut (incision) in your abdomen during the procedure. This allows the surgeon to see your internal organs. Instruments are then inserted through other small incisions in your abdomen or vagina to remove your uterus, cervix and any other parts of your reproductive system. These laparoscopic surgeries are usually carried out using general anaesthesia, where you'll be unconscious during the procedure.
Who is it usually recommended for?
Laparoscopic surgery is also known as keyhole surgery. It's the preferred way for most patients to remove the organs and surrounding tissues of the reproductive system.
Healing and Recovery
This method is the most common since it is the least invasive. Therefore, it has a shorter hospital stay and faster recovery time. There is also generally less pain and bleeding after the operation and reduced scarring relative to abdominal surgery.
Vaginal Surgery
How it works
During a vaginal hysterectomy, the uterus and cervix are removed through an incision that's made at the top of the vagina. Special surgical instruments are inserted into the vagina to detach the uterus from the ligaments that hold it in place. After the uterus and cervix have been removed, the incision will be sewn up. The operation usually takes about an hour to complete. A vaginal hysterectomy can either be carried out using general anesthetic – where you'll be unconscious during the procedure.
Who is it usually recommended for?
A vaginal hysterectomy is usually preferred over an abdominal surgery as it's less invasive.
Healing and Recovery
Because this method is less invasive than abdominal surgery, it generally involves a shorter stay in the hospital, and recovery time tends to be quicker than that of abdominal surgery. There is also less scarring relative to abdominal surgery.
Laparoscopic Assisted Vaginal Surgery
This approach combines both techniques of a laparoscopic and vaginal approach. This may be the preferred approach for some gynecologists and has the same benefits as a purely laparoscopic approach.
Abdominal Surgery
How it works
During abdominal surgery, an incision will be made in your abdomen. It will either be made horizontally along your bikini line or vertically from your belly button to your bikini line. A vertical incision will usually be used if there are large fibroids (non-cancerous growths) in your uterus, or for some types of cancer. After your uterus and/or ovaries have been removed, the incision is stitched up. The operation takes about two hours to perform, and a general anesthetic is used.
Who is it usually recommended for?
An abdominal hysterectomy may be recommended if your uterus is enlarged by fibroids or pelvic tumors and it's not possible to remove it through your vagina.
Healing and Recovery
Abdominal surgery is the most invasive method, and may result in more delayed recovery times and scarring.
Further reading about different approaches and their relative risks and benefits: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC558455/
-
Oophorectomy (plus hysterectomy) is a major surgery; recovery can be complex. Being psychologically and physically prepared is key. You can help make it easier by preparing your home and organizing extra help in advance.
Fellow patients who had undergone the surgery kindly offered advice for preparing in advance, including Items For Recovery and Preparing Your Home for an easier recovery.
📌 Tip: You do not need to shave or wax your pubic hair, especially for surgery. You should avoid shaving pubic hair pre-surgery since any nicks in the skin from the razor can make you more vulnerable to infection. Gynecological surgeons see vulvas of all shapes, sizes, and hairiness every day, so you do not need to worry! Also, you can still have the surgery if you are on your period, so don’t worry if your op date falls when you are bleeding - they have seen it all before!
-
Yes! It is your body and ultimately your decision. You are entitled to change your mind even at the last minute. If you have concerns, it is best to discuss your reasons and worries with a trusted friend and doctor. Worrying about the surgery and the outcomes is exceptionally normal, but if you feel your worries are more than “last-minute jitters,” then ensure you speak to people who can help you. Do not let anyone push you into having major surgery if you feel it is not right (or not the right time) for you and your circumstances.
Short-Term Recovery
Most people have questions and concerns about how they will feel when they wake up from surgery and about recovery in the first few weeks. We will cover some of the basics here.
-
This will vary from person to person. Waking up from anaesthetic can be a daunting experience, especially if you have not had surgery before.
Common experiences include:
Disorientation/Being Overwhelmed
Waking up from surgery can be disorienting and overwhelming. Gaining consciousness in unfamiliar surroundings can be confusing. It is common to feel emotional and teary upon waking up, so know that it is normal and you are not alone in experiencing this.
Nausea
The anaesthetic can make you nauseous, and it is not unusual to vomit when you awake. The nursing team will be used to this and will have sick bags/bowls available.
Trapped Gas Pain
During laparoscopic abdominal surgery, gas (commonly carbon dioxide) is used to ‘inflate’ the abdomen, giving the surgeon more room and a better view of the internal organs. Many report waking up with stomach and shoulder pain where the gas has moved post-op. Pain medication and gentle movement can help. This pain can last a few days.
Pain
Patients report varying levels of pain when waking up from surgery. For some, it is very minimal, and others have greater pain. Your care team will be able to provide appropriate pain relief, so be sure to tell them about your pain and ask for additional help in managing the pain as needed. Do not let the pain build up before requesting assistance.
Feeling Cold
It is common to feel very cold and have rigors (shaking due to coldness). This is usually due to the anesthetic inhibiting the body's capability to regulate temperature, although cutaneous vasodilation (triggered by post-operative pain) may also be a factor. Recovery nurses are trained to notice this and will provide blankets to keep you warm if needed.
-
This will vary depending on which type of surgery you had (e.g. laparoscopic or abdominal) plus (1) If there were any complications and (2) Which hospital you are having your surgery, as policy and procedure will vary across different facilities/health care systems.
Some people will go home the same day, while others will stay in the hospital for up to 3/4/5 nights. If there are no complications, you can ask your surgeon/care team how long you will be expected to remain in the hospital.
The average hospital stay for abdominal surgery (the most invasive option) in the US is around 3 days. For laparoscopic hysterectomy/oophorectomy in the US, most patients are discharged on the same day. However, the average in other countries will vary, so it is best to ask your surgeon in advance.
-
Urinating
You will likely be catheterized for surgery once you are under the anaesthetic. Catheterization is when a small, flexible tube is inserted into the urethra to drain urine from the bladder while you are unconscious.
The catheter is usually removed 12-24 hours after the surgery, and urination often returns to normal pretty quickly.
Defectating
Painkillers and anesthesia can make you constipated and so some people find they will need medication to help them poop after surgery. It can take a couple of days for a bowel movement to occur.
Avoid straining if you are constipated, as you will have multiple internal stitches that need to heal. Ensure you drink plenty of fluids when you wake up from surgery to help your bowels! If you have any concerns about not being able to pass urine/poop do seek help from a healthcare professional.
-
A small amount of vaginal bleeding (similar to a normal period) is not unusual for up to 6 weeks following surgery. In this case, you should use a sanitary towel and not tampons/menstrual cups.
You should not use any products that you have to insert into the vagina as this increases your risk of infection.
If you are experiencing more bleeding than a normal period or noticing any clots or abnormal-smelling discharge, you should visit a healthcare professional for a check-up to ensure there is no infection.
-
You will be able to shower quite soon after having surgery, within 12 to 24 hours.
Surgeons generally discourage taking a bath for the first several weeks.
It can be helpful to make sure you have a non-slip bath mat at home and have some help getting in and out of the shower initially. Try to avoid heavily scented products, which may aggravate any sensitive wounds.
-
Again, this will vary depending on which type of surgery you had (laparoscopic/abdominal) and how your recovery is going.
You should not drive a car until you can move easily and no longer require narcotic pain medications. Be mindful that you may have lots of internal stitches, so you need to be careful in case you are involved in an accident and cause internal damage.
Speak to your health care provider if you have questions. Some Car Insurance companies request that you call them for approval before driving.
-
This download, showing approximate recovery times for those who have had a Laparoscopic Total Hysterectomy with Bilateral Oophorectomy (the most common surgery for PMDD), is a must to print off. If you live with others, it can be wise to display it in a communal area (like on the kitchen fridge) so that they are all aware of your expected capabilities during your recovery.
Note: These timings are estimates and will be used as a general guide. Those who have had abdominal surgery or just an oophorectomy will have to adjust these times to their needs.
-
The timeframe will depend on a few factors: mainly, which type of surgery you had and which method of surgery was used (i.e., the invasiveness of the surgery). You may need longer to rest and heal. Recovery from laparoscopic (keyhole) surgeries will take less time to heal compared to an abdominal surgery. If you did not have a hysterectomy in addition to your ovary removal, you may find you need less time to recover.
It can also depend on your job role - it may take less time to return to work if you are desk-based, and may take more time to return to work if your job is manual and requires more physical effort. As well as speaking to your doctor, it may be helpful to speak to your HR department if you feel a phased return to work would be useful to you. As well as the physical healing, fatigue is common, and so it is important not to rush back to work before you feel capable of doing so.
Your rights to leave can also vary from country to country. For example, in the UK, 6 weeks is the average time granted for time off work to recover from a hysterectomy/THBO, and in the US, FMLA leave can be used (up to 12 weeks per year) as needed before you are able to return to work.
Rest as much as possible during this time and do not lift anything heavy, such as shopping bags. Your abdominal muscles, internal stitches, and tissues need time to heal.
-
This will vary from person to person and will depend on several factors. Those who are already on HRT pre-op may find that they don’t even have menopausal symptoms as their levels are kept at a reasonable level.
The dosage and timing of HRT should be discussed with your surgeon before the operation. Some doctors we surveyed reported that they prefer to begin HRT when the patient leaves the hospital (provided medical safety for the individual patient); however, there is no clear scientific guidance about when or at what level to start. Studies suggest that HRT is underused in surgical menopause, so it is essential to have discussions with your doctor before surgery about how you will work together to optimize HRT in surgical menopause.
Remember that you may also experience short-term emotional symptoms during this transition. Several studies show that people with PMDD experience abnormal, adverse emotional reactions during hormone changes. However, recent studies ALSO show that these adverse emotional reactions usually go away about one month after starting HRT. Therefore, if you can tolerate the symptoms in the first month following the start of HRT (or any changes in HRT), symptoms usually subside. So while it can be a difficult start, many women with PMDD can take HRT during surgical menopause.
If you’re concerned about your ability to cope with initial symptoms in the first month of HRT, we encourage you to start with a low dose and build up slowly. It is wise to be aware that this can be a difficult time with increased symptoms, and plan to expand support from family, friends, and healthcare providers during this time. For example, some people can start HRT during a “quiet month” where there is less stress in their lives. Some may also see a supportive health care provider more frequently during the first month of HRT, or ask those around them to provide additional support.
The First Year After Surgery
We often hear from people who are months/weeks (or even days!) post-op who are wondering why the surgery has not ‘fixed’ them. Surgery for PMDD is different from, say, having a tumour removed. It is not a case of removing the part, getting sewn up, and being done. The surgery is primary, and you are having part of your endocrine system removed.
PMDD is a sensitivity in the brain to hormonal fluctuations. For those with PMDD, it is essential to note that, although the removal of the ovaries prevents the monthly cyclical hormone fluctuations that may trigger brain reactions to hormones (e.g., emotional or cognitive changes), your brain will always be abnormally sensitive to hormones, and surgical treatment will not change that. The surgery takes away the primary source of the fluctuations (ovulation). Even those who do not have that hormonal sensitivity can struggle with the dropping hormone levels.
You cannot have PMDD when you no longer have a menstrual cycle, but you may feel PMDD-like symptoms when you have a fluctuation. Fluctuations can be caused by various actions (both natural and also by patient actions) including (but not only): natural depletion of hormones in the body as your levels drop, changes in HRT (raising and lowering dosage), drinking alcohol, missing a dose of HRT (or in some cases, applying/administering late).
Tracking your symptoms, alongside any lifestyle changes or medications, can help give you and your provider a clearer picture.
There is no one experience of how long it takes for the hormones to ‘settle’ so they are steady and level. Some patients report finding the proper HRT dosage early and keeping their levels steady. It’s a longer process for others, but equally as ‘normal’ an experience. Since it may take quite some time to find the optimal dosages of HRT, many people with a history of hormone sensitivity still experience changes in their symptoms during this process.
It does not mean that you still have PMDD - it just means that your brain is reacting to any fluctuations that are occurring, and some of these are out of our control whilst the body adjusts, so patience is key.
It should be noted that, in the case of PMDD, there is thought to be a time lag of about 2 weeks between hormone changes and brain reactions; therefore, frequent changes to HRT levels should be avoided, and every change should be evaluated for about one month before deciding if it is effective and tolerable. Tracking can be beneficial.