Premenstrual Disorders & Menopause
Menopause - the ceasing of menstruation.
Most of us living with PMDD and/or PME will be affected by menopause at some time in our life - whether it be our symptoms changing due to being in perimenopause, going through chemical menopause as part of a treatment plan, or, for those who have had no relief through other means, surgical menopause (which occurs when the ovaries are surgically removed). This page is to help you understand the different types of menopause (yes - there is more than one!) and how it may affect your health/symptoms in regard to having a Premenstrual Disorder.
Isn’t there just ‘one kind of menopause’ though?
You may be surprised to hear that no - menopause (the ceasing of menstruation) comes in a few different guises - some occurring naturally, and some as the result of a medication.
Understanding The Different Types Of Menopause
POI (Premature Ovarian Insufficiency)
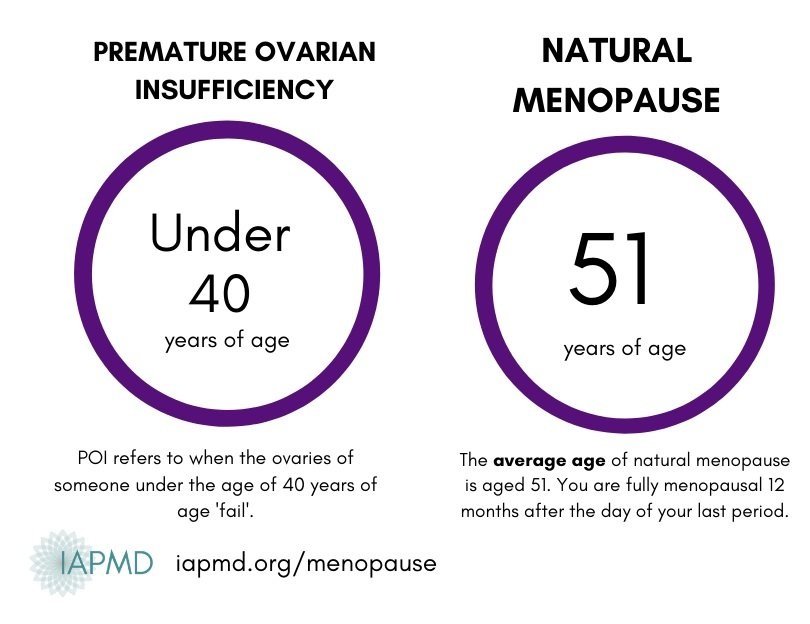
The term POI is reserved for those below the age of 40 whose ovaries are not functioning as they should. They are unable to produce estrogen, progesterone, and testosterone in adequate amounts, and infertility, menopausal symptoms, and associated health risks (e.g. early heart disease, osteoporosis) can result.
What causes POI?
POI can occur for a number of reasons including chemo/radiotherapy, infection, or genetic factors; however, the cause is often unknown. POI may also be termed premature menopause, but it is not always “menopause” in the true sense as the ovarian function can fluctuate and may return temporarily (however, this is rare).
Those who undergo premature surgical menopause and those who experience POI as a result of other factors do have things in common: They may experience similar symptoms associated with an ovarian hormone deficiency, and difficulties relating to psychological adjustment of their diagnosis. If menopause occurs between the ages of 40 and 45, this is referred to as early menopause. At least one in a hundred will experience menopause under the age of 40 – this is referred to as premature menopause or premature ovarian insufficiency (POI).
How Do I Know If I Have POI?
If you are under 40 and have noticed a change in your menstrual cycle (i.e. your periods have become irregular or have stopped altogether), and/or believe you are experiencing (peri)menopausal symptoms (e.g. hot flushes, mood changes, joint pains, vaginal dryness), you will need to have a blood test to measure the level of a hormone called follicle-stimulating hormone (FSH). If the FSH level is raised then this blood test will need to be repeated in 4-6 weeks.
The recommended diagnostic criteria for POI include irregular or no periods for at least 4 months, and an elevated FSH level (<25 IU/L) on two occasions at least 4 weeks apart. See here for further details.
How would POI affect PMDD/PME?
As spontaneous POI (i.e., POI that occurs “naturally”, and not as a direct result of medical or surgical treatment) leads to irregular cycles (before periods cease altogether) this will increase hormonal fluctuations. This can lead to an increase in symptoms, as well as unpredictable patterns. However, once periods have fully stopped, PMDD/PME symptoms tend to vastly reduce (as there are no further menstrual cycles to trigger symptoms).
Having said that, most individuals who experience POI will require HRT to protect their long-term health, and this can lead to symptom resurgence as a result of hormone sensitivity when starting treatment and/or as a result of any further treatment changes. The good news is that most women and AFAB individuals with PMDD tend to adjust to new HRT changes after 4-6 weeks.
Perimenopause & Natural Menopause
Perimenopause - Natural menopause occurs after a transition period (which can last from months to years) called perimenopause where the body gradually makes less estrogen to a point where the ovaries stop releasing eggs (menopause).
Natural menopause - occurs when the ovaries stop releasing eggs and, as a result, the levels of sex steroid hormones (estrogen, progesterone, and testosterone) fall. The average age of natural menopause is 51 years of age (although this can vary between different ethnic groups), but any time after 45 is considered ‘normal.’ The years during the menopausal transition are called perimenopause, which can last months or even up to years. Periods often become heavier and more sporadic during this time, and menopausal symptoms (e.g., night sweats, hot flashes, or vaginal dryness) begin to appear.
It's worth talking to your doctor if you have menopausal symptoms that are troubling you or if you're experiencing symptoms of menopause before 45 years of age.
They can usually confirm whether you're menopausal based on your symptoms, but a blood test to measure your hormone levels may be carried out if you're under 45.
How may being perimenopausal affect my PMDD/PME?
PMDD cycling does go away after you are fully menopausal; however, during the years before and during the menopause transition (perimenopause), things can get rough for a while since those with PMDD are sensitive to hormone changes, and hormone flux increases EVEN MORE during perimenopause. Estrogen and progesterone production becomes very erratic and unstable before it declines at menopause.
Are there any treatments to help?
Hormone replacement therapy (HRT), in those able to take it, can help smooth out the hormonal fluctuations of perimenopause and improve both symptoms of estrogen deficiency and PMDD. However, as those with PMDD are inherently sensitive to any new hormonal changes it can take a few weeks for things to settle, so please bear this in mind.
SSRIs can also be beneficial in managing worsening PMDD symptoms during perimenopause as they can help to stabilize neurotransmitters in the brain (therefore, reducing PMDD and mood-related symptoms).
How Do I Know If I Am Postmenopausal?
If you are going through menopause naturally, you will be considered postmenopausal a year to the day of your last period. PMDD cycling does go away after you are fully menopausal. However, those with PMDD have a sensitivity to hormone fluctuations - you may still experience PMDD-like symptoms when starting (or changing dosage) of HRT. Several studies show that people with PMDD experience abnormal negative emotional reactions during hormone changes. However, recent studies ALSO show that these negative emotional reactions usually go away about one month after starting HRT. Therefore, if you can tolerate the symptoms in the first month following the start of HRT (or any changes in HRT), symptoms usually subside.
Any vaginal bleeding after you are postmenopausal should be investigated with a healthcare professional. This advice stands even if bleeding occurs once, if there's only a small amount of blood, spotting, or pink or brown discharge, you do not have any other symptoms or if you're not sure if it’s blood.
Postmenopausal bleeding is not usually serious but can be a sign of cancer. Cancer is easier to treat if it's found early.
Chemical Menopause
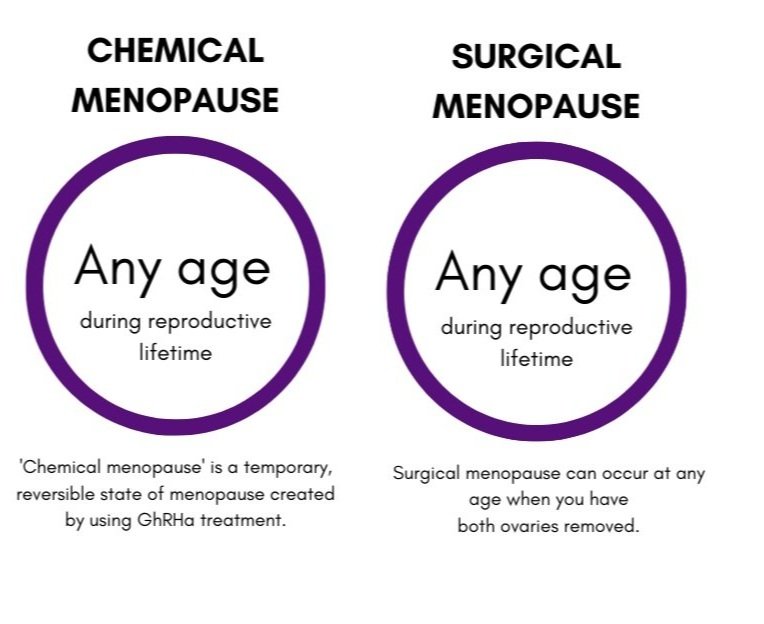
Gonadotropin-releasing hormone analogs (GnRH analogs or GnRH agonists) are a treatment that is sometimes used to treat PMDD. These drugs act by suppressing the estrogen production by the ovaries by inhibiting the secretion of regulatory hormones from the pituitary gland. As a result, your natural hormone levels drop low and therefore your menstrual cycle stops, mimicking menopause - it is often referred to as ‘Chemical Menopause’. This is a temporary and reversible state it is often used before surgery, to ensure the accurate diagnosis of PMDD and also to make sure you tolerate HRT as this is an important consideration before surgery.
How Will I Feel When I Start This Treatment?
This experience will differ from patient to patient. Some people will feel better right away - their ovaries will shut down quickly, they have minimal symptoms from this ‘shut down’ and they start HRT with minimal issues. For others, it will take 2 /3 months for the GnRHa agonists to suppress the menstrual cycle. By shutting down the ovaries you are put into a menopausal state - and many symptoms of menopause can feel a lot like PMDD! Some may experience undesirable side effects. Most commonly these may include hot flushes, reduced sex drive, headaches, mood changes including depression, vaginal dryness, and change in breast size. These symptoms mean the medication is working and is not a reason for discontinuation. HRT is used to counteract the low level of hormones and if you are feeling these symptoms then your dose of addback estradiol will need adjusting.
In these first weeks, it is common to have a ‘flare’ in hormone levels, and therefore you may experience PMDD - like symptoms, as your brain adjusts and downregulates its hormonal stimulation to your ovaries.
To read more about GnRHa Treatment, you can visit our extensive resource here:
Surgical Menopause
Some of those who have not gained adequate relief from other treatments/methods, choose to go on to have surgery for PMDD. Surgery is the last line in treatment for premenstrual disorders reserved for those who have not gained relief through other evidence-based treatments. Surgery involves removal of the ovaries and often the uterus, which induces menopause and is called surgical menopause. There are many factors to weigh when considering surgical menopause as a treatment for PMDD/PME, including medical eligibility, the likelihood of treatment success, and personal preferences.
In those who undergo bilateral oophorectomy (removal of both ovaries), the transition into menopause is immediate and known as surgical menopause. The symptoms can be sudden and may be more intense than those experienced in natural menopause, especially in younger individuals.
How Do I Know If I Am In Surgical Menopause?
You will enter surgical menopause as soon as you have both of your ovaries removed.
Can You Still Have PMDD If You Are In Surgical Menopause?
No. No ovaries = No ovulation = No fluctuations = No PMDD. Removal of the ovaries (oophorectomy) is permanent and means that your body will naturally be in a menopausal (low hormone) state for the rest of your life.
If you have just had a hysterectomy (and not a bilateral oophorectomy) you can still have PMDD post-surgery as the ovaries will still be functioning.
If you have had both ovaries removed for the treatment of PMDD, it is important to note that, although the removal of the ovaries prevents the monthly cyclical hormone fluctuations that may trigger brain reactions to hormones (e.g., emotional or cognitive changes), your brain will always be abnormally sensitive to hormone fluctuations, and surgical treatment will not change that. You are likely to still feel negative emotional reactions to any fluctuations caused by situations such as natural hormone depletion, HRT not absorbing properly, and changes in HRT levels/delivery methods. The aim is to get your levels steady with adequate HRT and keep them at that rate so there are no fluctuations to cause symptoms.
Since it may take quite some time to find the optimal dosages of HRT, many people with a history of hormone sensitivity still experience changes in their symptoms during this process. It does not mean that you still have PMDD - it just means that your brain is reacting to those fluctuations that are caused by a change in HRT, the natural depletion of hormones from your body, or the HRT not being correctly absorbed.
It should be noted that, in the case of PMDD, there is thought to be a time lag of about 2 weeks between hormone changes and brain reactions; therefore, frequent changes to HRT levels should be avoided, and every change should be evaluated for about one month before deciding if it is effective and tolerable.
Have other questions? Don’t forget that our FAQ knowledge base is packed full of your questions with answers from experts!
If you are considering, preparing for, going through, or recovering from surgery for PMDD, we recommend spending some time viewing our extensive resource on surgery and surgical menopause for PMDD:
With thanks to Dr. Hannah Short (PMS & Menopause Specialist) for her input and assistance in collating the information on this page.