Estrogen Therapy in Surgical Menopause
If you have kept your uterus (that is, you have NOT had a hysterectomy), it is generally unsafe to take estrogen without a progestogen (sometimes referred to as “unopposed estrogen”) since it can cause a cancerous overgrowth of the uterine lining. However, taking progestogen therapy (which comes in many forms) at the same time will prevent this overgrowth and make estrogen therapy safe for long-term use. Keep in mind that menstrual bleeding or spotting is not a good indicator of whether or not the uterine lining is becoming too thick; only an ultrasound can diagnose this overgrowth. On the other hand, many trials have demonstrated that a variety of progestogen options are effective for preventing overgrowth.
If you have had your uterus removed (hysterectomy) in addition to your ovaries, estrogen can be taken alone and you will not need progestogen ‘add-back’ to protect your uterus.
What is estrogen? (Alternative spelling: Oestrogen)
How does surgical menopause influence estrogen levels?
Why is Estrogen Therapy needed?
When should I start using estrogen therapy? At what age/stage should you stop using it?
What are the different methods of taking estrogen? Are some better than others?
Are there any alternatives to estrogen in surgical menopause?
Don’t forget to check out the IAPMD knowledge-base for lots of answers to your questions here.
To read more about the benefits and risks of HRT in surgical menopause:
What is estrogen? (Alternative spelling: Oestrogen)
Estrogen refers to a group of hormones in the body (estradiol, estrone, estriol) that function as the primary female sex hormones. Estrogens are responsible for the development and regulation of the female reproductive system, but they also play critical roles in the health of other systems, including the heart and vasculature, bone, the vulva and vagina, and the brain (that is, maintaining stable mood and ability to think clearly and remember things). Estradiol (E2) is the most common and potent estrogen in the body. Estrone (E1) is another important estrogen that has potent effects primarily because it is converted to estradiol in the body.
Estrogen therapy (ET) is available in many different forms and dosages by prescription. Typically, ET includes estradiol, although sometimes it includes estrone (a precursor molecule that causes your body to make its own estradiol) or estriol. When the uterus has been removed (bilateral oophorectomy WITH hysterectomy), estrogen can be taken alone. When the uterus remains, estrogen must be taken along with a progestogen to prevent cancer of the uterus.
How does surgical menopause influence your estrogen levels?
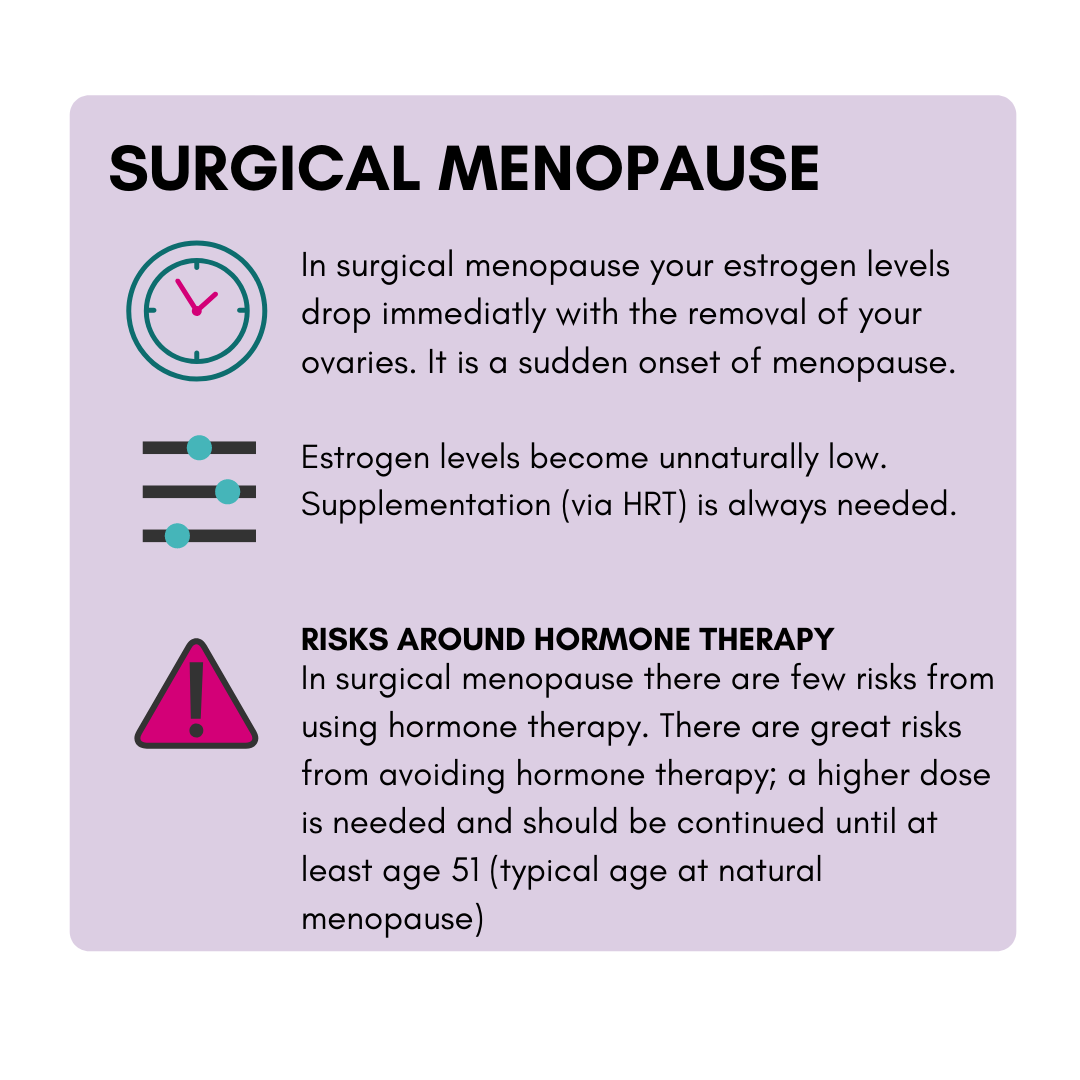
When you have both ovaries removed (bilateral oophorectomy/surgical menopause), you remove your body’s main source of estrogen, and your estrogen levels will plummet lower than in natural menopause. These extremely low levels of estrogen are thought to be the main cause of both bothersome menopausal symptoms and long-term health risks in surgical menopause. Thankfully, taking estrogen in surgical menopause reduces both.
Why is Estrogen Therapy needed?
Following a bilateral oophorectomy (both ovaries removed), the patient immediately enters surgical menopause, meaning that they become postmenopausal right away. Although there are some similarities between natural and surgical menopause, the needs for estrogen-therapy are far greater in surgical menopause, and typical guidelines for HRT often do not apply in surgical menopause. This is because, relative to natural menopause, surgical menopause causes a faster hormone drop and lower overall levels of hormones in the long term.
The ultra-low levels of estrogen in surgical menopause can cause bothersome menopausal symptoms, but more importantly, they can reduce the length and quality of your lifespan by increasing risk of various serious health conditions. We will address each below.
HRT in surgical menopause reduces or eliminates bothersome menopausal symptoms, including:
vasomotor symptoms (for example, hot flashes or night sweats with sleep disturbance)
musculoskeletal symptoms (for example, joint and muscle pain)
effects on mood or anxiety (for example, feeling abnormally sad or worried)
urogenital symptoms (for example, vaginal dryness)
sexual difficulties (for example, low sexual desire).
For those under the age of 40 entering surgical menopause, using estrogen-therapy also reduces or eliminates the serious long-term health risks associated with surgical menopause, including:
osteoporosis and broken bones
cardiovascular disease (for example: heart attack, stroke)
dementia and Parkinsons disease
psychiatric disorders (for example: mood or anxiety disorders)
vulvar and vaginal atrophy
sleep disorders (for example: persistent and impairing insomnia)
higher risk of death by any cause
To summarize, surgical menopause is known to cause all of the above symptoms and health risks-- but these problems can generally be reduced or eliminated by using estrogen therapy following surgery through to the typical age of menopause (51 years). Most individuals in surgical menopause choose to continue some level of estrogen through at least age 60 to maintain symptom relief.
HRT can be taken quite safely by the vast majority of people in surgical menopause. See this section for a discussion of risks, including potential concerns of those with familial cancer or blood clot risk or hormone-sensitive mood symptoms (e.g., Premenstrual Dysphoric Disorder or PMDD).
The type of HRT most suitable for you will depend on a variety of factors, including whether or not you had a hysterectomy as well as ovary removal (bilateral oophorectomy).
For more information about the specific hormones used in HRT (estrogen, progestogens, and testosterone), including methods of taking them (patches, gels, pills, etc.), and instructions for monitoring appropriate dosages, can be found via the main page here.
References:
NAMS 2017 Hormone Therapy Position Statement (North America)
When should I start using estrogen therapy? At what age/stage should you stop using it?
Experts recommend beginning estrogen immediately following surgery and continuing until the typical age at natural menopause (around 51 years old) in order to protect bone, brain, and cardiovascular health. However, many individuals continue to safely use estrogens after this time, and some guidelines recommend continuing through age 60.
How long does estrogen take to work? How long should I try out a certain dose before making a change?
Estrogen therapy can take up to two weeks to work, and temporary side effects can take several months to dissipate (although some can be persistent!). We recommend tracking your symptoms and side effects daily (or at least weekly) in order to have a clear visual of how symptoms are responding, and whether side effects are decreasing over time.
Similarly, any changes made to your therapy route, dosage or frequency should be noted in your daily/weekly tracking document/app so that the pattern of change can be monitored objectively. We recommend waiting at least one full month on the new therapy before evaluating the new treatment or making any additional changes, since effectiveness and side effects may fluctuate prior to stabilizing again on the new treatment.
This is particularly important for those who have an emotional hormone sensitivity; studies suggest that any change in hormone levels can provoke symptoms among those patients, but that those symptoms go away again after one month of the new therapy. Therefore, patience and support are needed to evaluate the “true” effects of any treatment change.
What are the different methods of taking estrogen? Are some better than others?
Several expert guidelines for hormone therapy in premature menopause (ACOG-POI; ACOG-young POI, BMS-POI) recommend starting with the use of transdermal or oral estradiol therapy in order to mimic the natural pre-menopausal state as closely as possible. However, a variety of other routes are available. Existing studies indicate that all estrogens (with the exception of locally-acting vaginal estrogen products) are effective for protecting against health risks and managing bothersome menopause symptoms.
The two most common (and recommended) forms of hormone therapy are transdermal estradiol (patches or pills) and oral micronized estradiol.
Transdermal estradiol (estrogen that is delivered through applying to the skin in either a gel or patch form).
Expert guidelines for the management of premature menopause (ACOG-POI; ACOG-young POI, ACOG-Prescribing for POI; BMS-POI) recommend beginning with transdermal estradiol because it has a more positive impact on clotting factors lipids, inflammation, and blood pressure (which may improve safety if continued after the typical age at menopause (i.e., 51)). The transdermal route is especially recommended for those who have elevated risk of blood clot due to other risk factors (most notably an elevated BMI or smoking). Transdermal estradiol is available in the form of patches placed on the hip or buttocks (USA or UK), or gels that are placed on the arms (primarily UK). Some evidence suggests that the gel produces fewer local skin irritations than the patch.
Oral micronized estradiol (estrogen that is delivered by taking a pill/tablet orally).
Estrogen is available in many different pill forms however, the most commonly used preparation is oral micronized estradiol. Among women and AFAB individuals who are in natural menopause, there is evidence that, relative to transdermal approaches, oral estradiol is associated with greater increases in risk for blood clots and unhealthy lipid changes. However, the absolute risks remain small, and oral estradiol a safe option for those in surgical menopause if transdermal methods are not tolerated.
What can I show my doctor to educate them about the importance of estrogen therapy in surgical menopause?
We recommend sharing any of the following resources with your doctor:
The American Journal of Obstetrics and Gynecology (ACOG) Committee Opinion on Hormone Therapy in Primary Ovarian Insufficiency (Specifies Recommended Hormone Dosages)
The North American Menopause Society (NAMS) Hormone Therapy Position Statement
Are there any alternatives to estrogen in surgical menopause?
In the case of breast cancer, studies suggest that estrogen does not increase risk of breast cancer when used in surgical menopause, even among those who are BRCA1 or BRCA2 carriers provided they do not have a personal history of cancer. In those in surgical menopause who have a Factor V Leiden mutation (which increases risks for blood clots), the long-term protective effects of hormone therapy may often outweigh the risks posed by the use of hormones.
Nevertheless, if you are concerned about using estrogen due to a family history of estrogen-dependent cancers, blood clots, or other risks, it is wise to discuss this with your doctor to make sure that you are carefully dosed and monitored to avoid adverse effects of hormones in surgical menopause. Alternative medications can also be used in some extreme cases (e.g., in patients with current estrogen-positive cancers).”
Estrogen therapy is the most effective way to prevent all of the symptoms and risks associated with surgical menopause. However, for those who absolutely cannot take estrogens, there are some alternative therapies available:
For hot flashes and other vasomotor symptoms, paroxetine is FDA approved, and other drug approaches may be effective (other SNRI/SSRI antidepressant drugs, clonidine, and gapabentin)
For depression, desvenlafaxine is the only medication that has been shown to be effective in large trials in menopausal depression, although other antidepressant medications and cognitive behavioral therapy may also be effective.
For vaginal dryness and atrophy, effective alternatives include low-dose vaginal estrogen cream, prasterone, and ospemifene; additional helpful approaches include vaginal lubricants, moisturizers, and laser therapy.
For osteoporosis, effective alternatives include biphosphenate medications and selective estrogen receptor modulators such as raloxifene, tamoxifen, or bazedoxifene+estrogen.
If you kept your uterus and need information on progesterone add-back, you can read more here: